On Thursday. April 16, Rabin Martin, as the Secretariat for the Private Sector Roundtable for Global Health Security (PSRT), hosted an eighth call in a series on the latest health impacts of COVID-19. The call featured two experts on the COVID-19 situation in Africa.
Dr. John Nkengasong, Director, Africa Centers for Disease Control and Prevention, reported that there are currently 18,000 cases among 52 countries on the African continent – a 6 percent increase since last week – and that deaths are approaching 1,000. While those numbers may not seem as high as expected, he noted that the situation can change very quickly as it did in the U.S. and U.K. He emphasized that it’s dangerous to talk about flattening the curve: “This is a treacherous virus. If you become complacent, you will be in deep, deep trouble.”
Dr. Nkengasong briefly described a new continental strategy that 36 Ministers of Health agreed to following an emergency meeting convened by the African Union in February. The three pillars are 1) limiting transmission, 2) limiting deaths and 3) limiting harm.
The Africa CDC is supporting countries in the following areas: scaling up diagnostics; training on infectious disease control; surveillance and screening; risk communication; and commodities distribution. Dr. Nkengasong asked that the private sector consider supporting countries either on a bilateral basis or more broadly through a new Africa COVID-19 Response Fund, a partnership with the African Union. Reflecting on the global nature of the pandemic (as opposed to localized Ebola outbreaks), he asserted that this is a global fight: “COVID-19 will not be declared over anywhere unless it is declared over everywhere in the world.”
Dr. Githinji Gitahi stated that the response to COVID-19 has to be “government-led and community-owned.” He emphasized that people need to understand what social distancing means across the diversity of community contexts in Africa. The government imposing a lockdown and expecting people to obey is unlikely to be effective unless communities understand the potential impact of the crisis on their daily lives and own their response.
He added that the private sector has played an important role in the response – from setting up hand washing stations in areas where there is a lack of water, or donating advertising space (billboards, radio and TV spots) to the government for public service announcements, to supporting a “FlexiFund” to enable the quick purchase of items that the government does not have on hand or is unable to make.
Dr. Gitahi also highlighted the “interdependency” of global health security and universal health coverage. He noted the disturbing trend of people hiding COVID-19 symptoms because of the financial implications of testing positive. In some countries, individuals pay for the cost of being quarantined and the care needed. In addition, people do not want to be prevented from working and losing income. He added that removing financial protection, especially for the most vulnerable, will hinder access to care, which will have a dire impact.
“If the response is not managed properly, economies will fail given the informality of the economy in Africa, with many people losing jobs, salaries cut and daily wage-earners unable to work.” Both speakers noted that COVID-19 must be viewed as an acute infection – “If it is chronic, we will not survive because we cannot continue to lock down economies.” They noted that there is a double-edged sword to the response: a strong need to support people’s health, but the danger of reducing taxes to mitigate the economic impact of the pandemic. Summarizing this challenging situation, Dr. Gitahi posed the questions: “When is the curve flat enough? What is the cost of a flatter curve? At what point is the cost of flattening the curve too much?”
John Nkengasong reminded everyone of what’s at stake in his closing remarks: “We have to win this fight for the continent to survive.” With a strategy of coordination, collaboration, communication and partnership – with both the private sector and civil society – Africa is planning to win.
Pandemic Spread

Severe mobility restrictions are helping to “flatten the curve,” but the virus continues to spread rapidly, hurtling the world past the inauspicious milestone of over two million cases. The U.S. has earned the unfortunate title of having the largest number of deaths (31,002) attributed to COVID-19, surpassing China where the virus first took hold three months ago. There are now 640,014 reported cases of COVID-19 in the U.S., accounting for nearly a third of the global burden. Worldwide, as of Thursday, April 16 at 9:00am ET, the Center for Systems Science and Engineering at Johns Hopkins University reported 2,088,425 confirmed cases and 139,419 deaths attributed to COVID-19.
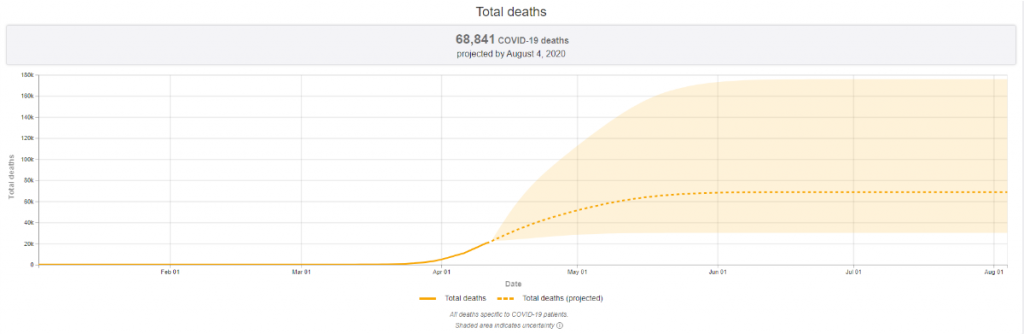
Experts say that widespread testing and contact tracing will be instrumental to reeling in viral spread. Updated models by the Institute for Health Metrics and Evaluation show the epidemic in the U.S. is slowing, but leveling off at a very high rate. Predictions have increased the estimated death toll to 68,841, up from last week’s projection of 60,415. Although these projections reinforce the importance of maintaining strong public health countermeasures to mitigate the spread of the virus and flatten the curve of new infections, President Trump is now arguing for opening the U.S. economy within weeks. Moving too quickly creates a real risk of making it possible for the rate of infections and hospitalizations to accelerate. As the University of Minnesota’s Michael Osterholm has often observed, “We’re only in the first inning of a nine-inning game.” Health experts – and most state governors, who are on the front lines of the fight – agree that trying to re-open the economy prematurely may have the unintended consequence of re-igniting transmission.
This week proves once again that COVID-19 does not discriminate. Whether you are a frontline health worker or a political leader, you are at risk for contracting COVID-19. On Monday, April 13, U.K. Prime Minister Boris Johnson was released from hospital and is continuing his recovery from COVID-19. In a video message, he thanks the National Health Service for saving his life, calling the agency “this country’s greatest national asset.”
Industry Developments
Responding to calls to lead the global response with unity and solidarity, global stakeholders are pursuing novel collaborations to accelerate research and development of COVID-19 treatments and vaccines. On Monday, April 13, a group of scientists, physicians, funders and manufacturers convened by WHO announced their commitment to working together to develop a COVID-19 vaccine.
-
Initial data released on Monday, April 13, suggests that remdesivir, Gilead’s investigational COVID-19 treatment, is highly effective in inhibiting a key enzyme involved in the coronavirus replication mechanism. Results from Phase 3 clinical trials on patients with severe disease are expected in late April.
-
Merck KGaA announced on Tuesday, April 14, that it used its manufacturing platforms to re-engineer the manufacturing process for the Jenner Institute’s COVID-19 vaccine candidate and shorten the cycle from one year to two months. Large-scale manufacturing is critical to providing sufficient product for use in current clinical trials and for global consumption if the vaccine proves efficacious.
-
On Tuesday, April 14, two leading global vaccine manufacturers, Sanofi and GSK, announced a collaborative effort to develop a COVID-19 vaccine. Combining Sanofi’s recombinant-based COVID-19 vaccine candidate with GSK’s adjuvant technology, the partnership aims to create an effective vaccine that can be manufactured at scale.
-
On Wednesday, April 15, Abbott announced it is launching a third test, a laboratory-based antibody blood test, to detect COVID-19 infection. Shipping is set to begin this week with the aim of distributing 4 million tests in April – and 20 million tests per month going forward – in the U.S.
“We ask that governments and institutions currently financing or contributing to the development of drugs, vaccines or technologies for COVID-19 agree from the outset in their contracts with industry to the sharing of intellectual property rights…We are talking about sharing, not giving up.”
“We know we need to find something fast, because the impact of COVID-19 is so big. It goes beyond. It is about sharing clinical trial data. It’s even talking about sharing and increasing manufacturing capabilities: ramping up capabilities for testing, manufacturing of vaccines, once we have one, or of medicines. This is something that, at this scale, has never happened before.”
Thomas Cueni, Director General, IFPMA
From the Experts
“WHO wants to see restrictions [on social mobility] lifted as much as anyone. At the same time, lifting restrictions too quickly could lead to a deadly resurgence.”
Dr. Tedros Adhanom Ghebreyesus, Director-General, WHO
Friday, April 10
“Behind every death is a friend, a family member, a loved one. As a city, it is part of the healing process to be able to grieve and mourn for all those [who] have passed because of COVID-19.”
Dr. Oxiris Barbot, Commissioner,
New York City Department of Health and Mental Hygiene
Tuesday, April 14
“It is increasingly clear that the world’s response to this pandemic will not be effective unless it is also equitable. We have a responsibility to meet this global crisis with global solidarity. In addition to contributing to the development of diagnostics, therapeutics, and vaccines, these funds will support efforts against COVID-19 in low-and-middle-income countries.”
Melinda Gates, Co-founder, Bill & Melinda Gates Foundation
Wednesday, April 15
Additional Resources
Reports from International Governments and Bodies
- WHO COVID-19 Information and Guidance
- WHO Situation Reports, April 13, April 14, April 15
- White House Coronavirus Task Force Press Briefings, April 13, April 14, April 15
- CDC Coronavirus Resource Page
- COVID-19 Health Systems Response Monitor
- NCD Alliance COVID resources relevant to NCDs
Funding and Policy Trackers
- International Monetary Fund Policy Tracker
- Kaiser Family Foundation Coronavirus Policy Tracker
- U.S. Chamber of Commerce Foundation Corporate Aid Tracker
- Devex Interactive Funding Tracker
Resource Pages and Market Research Literature
- JAMA Resource Center
- The Lancet COVID-19 Resource Centre
- PharmaIntelligence: Coronavirus – What will the Impact Be?
- Health Affairs Resource Center
- STAT Preparedness Tool
Communications Toolkits