A conversation with Don Darden, General Manager of Firestone, Liberia, Inc.
On Tuesday, April 7, Rabin Martin, as the Secretariat for the Private Sector Roundtable for Global Health Security (PSRT), hosted a seventh call in a series on the latest health impacts of COVID-19. Don Darden, General Manger, Firestone, Liberia, Inc., reflected on the company’s response to the Ebola epidemic in Liberia in 2014 and compared it with preparations for COVID-19. To date, there are an estimated 7,646 confirmed COVID-19 cases in Africa, with the numbers expected to increase rapidly.

As the largest private employer in Liberia, with nearly a 100-year history operating in the country, Firestone plays a significant role in the health and safety of the 120 communities where its 7,500+ employees live and work. Darden described the agility the company demonstrated in the face of government bureaucracy when “the health system came to its knees” during the Ebola outbreak six years ago. For example, Firestone’s engineering team put up buildings and septic systems to isolate and care for Ebola patients, turned a gymnasium into a makeshift warehouse facility, and used its voice and clout to educate community leaders about protecting themselves and to help fight the stigma surrounding the disease.
In making the comparison with COVID-19, Darden stated that the situation is completely different – including Liberians’ reactions. He noted that unlike Ebola, “if they can’t see it, they don’t believe it” and, as a result, Liberians are not taking as many precautions to prevent COVID-19 as they should. He commented on the resistance to restricting people’s mobility as part of a lockdown, given common practices of congregating in marketplaces and elsewhere; high rates of illiteracy also make communicating about health threats more challenging.
While there have been only 14 confirmed cases of COVID-19 in Liberia so far (likely under-reporting), Darden noted that Firestone’s preparedness mentality has enabled the company to mobilize quickly even though there is limited access to resources in high demand in COVID-19 hotspots.
COVID-19 & LMICs: A Question of When
A burgeoning crisis
“This pandemic is a health crisis. But not just a health crisis. For vast swathes of the globe, the pandemic will leave deep, deep scars. Without support from the international community, we risk a massive reversal of gains made over the last two decades, and an entire generation lost, if not in lives then in rights, opportunities and dignity.”
Achim Steiner, UNDP Administrator
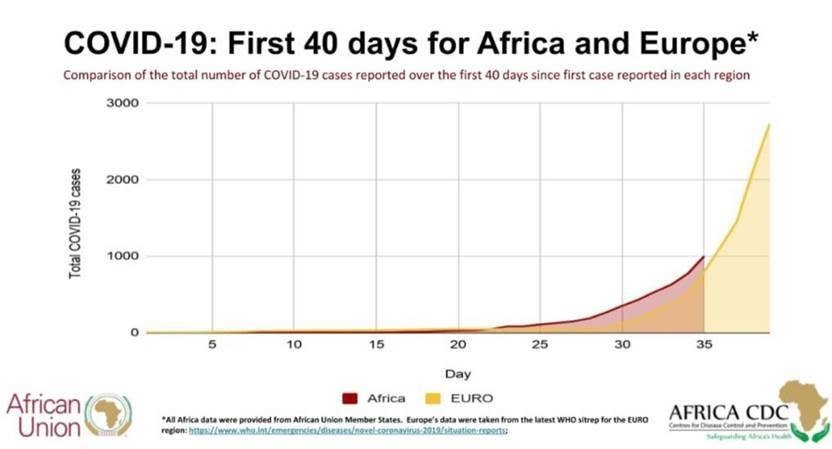
According to official estimates, LMICs are currently shouldering less of the global COVID-19 burden. While cases to date have been relatively low compared with the rest of the world (potentially due to lack of testing), the World Economic Forum notes that Africa has a veritable “COVID-19 time bomb to defuse.”
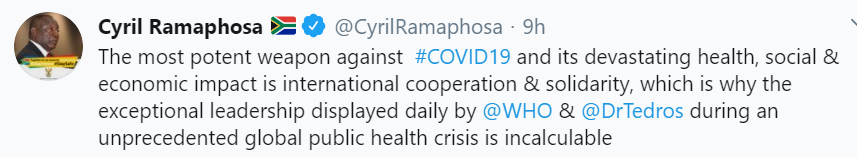
Although the United Nations has launched a $2 billion emergency response plan for LMICs, this is a fraction of what will be required, given that these countries have been described as “likely the next battlefield for the virus.” While certain countries, like South Africa, have implemented strict social distancing policies, it is not a realistic option for most, given large population segments required to leave their homes to sell goods, get water and food, etc. to meet basic needs. Also, with only two ICU beds per 100,000 people in India, Pakistan and Bangladesh (and even fewer in sub-Saharan Africa), COVID-19 could devastate already fragile health systems.
Ensuring LMICs are not left behind: Global actors respond
On Thursday, April 2, a group of over 70 global organizations, including the Bill & Melinda Gates Foundation, Wellcome Trust and several research institutes based in Asia, Africa and Latin America, launched the COVID-19 Clinical Research Coalition. The Coalition aims to accelerate COVID-19 research in resource-limited settings, bringing together individuals and institutions working to fast-track research that will provide evidence on COVID-19 prevention, diagnosis and case management.
A critical concern is ensuring that all research is conducted ethically, respecting the dignity of participants. On Tuesday, April 7, global actors, including the WHO, condemned racist comments from French scientists about using Africa as a potential testing ground for potential COVID-19 treatments, citing the region’s general lack of infrastructure.
On Friday, April 3, the Medicines Patent Pool announced the temporary expansion of its mandate to include “any health technology that could contribute to the global response to COVID-19 and where licensing could facilitate innovation and access.” Generic licensing of novel technologies to fight COVID-19 would support the response efforts of LMICs, ensuring their populations have access to affordable medicines and vaccines. This commitment builds on Unitaid’s announcement to commit an initial US$30 million for innovative treatment, diagnostics and respiratory triage tools as part of the global response to the pandemic.
On Monday, April 6, Dr. Tedros endorsed Costa Rica’s proposal for a pool to ensure full access to medicines and vaccines that are being developed to combat COVID-19, noting: “I call on all countries, companies and research institutions to support open data, open science and open collaboration so that all people can enjoy the benefits of science and research.”
Aid Effectiveness in the Age of COVID-19
The United Nations Conference on Trade and Development (UNCTAD) recently published an analysis of the potential economic shocks of COVID-19 on the economies of LMICs. The report calls for a “whatever it takes” approach to mitigate the pandemic’s effects on the “two-thirds of the world’s population being left behind.” UNCTAD brings attention to the potentially catastrophic economic impacts of COVID-19 for vulnerable economies, noting that it is “a matter of immediate urgency for the international community to co-ordinate appropriate economic rescue packages… to address the looming financing gap which many developing countries are now imminently facing.”
On Monday, April 6, the Modernizing Foreign Assistance Network hosted a virtual roundtable discussion on the COVID-19 response, global health security and implications for aid effectiveness. Rabin Martin CEO Jeff Sturchio offered some reflections on the need for an integrated approach to this issue – health and development are inextricably linked, as the COVID-19 pandemic demonstrates. Jeff recommended viewing the COVID-19 crisis from a global health security perspective and urged donors to ensure aid is allocated effectively to vulnerable countries to support the response. “The cost of baseline preparedness for prevention, detection, and response to emerging health crises is estimated at only about $1 per person per year, while the cost of inaction is measured in trillions,” Jeff said. “It is a global imperative for the international community to build resiliency in regions with fragile health systems so they can withstand the current pandemic and be ready for future health emergencies.”
Pandemic Spread

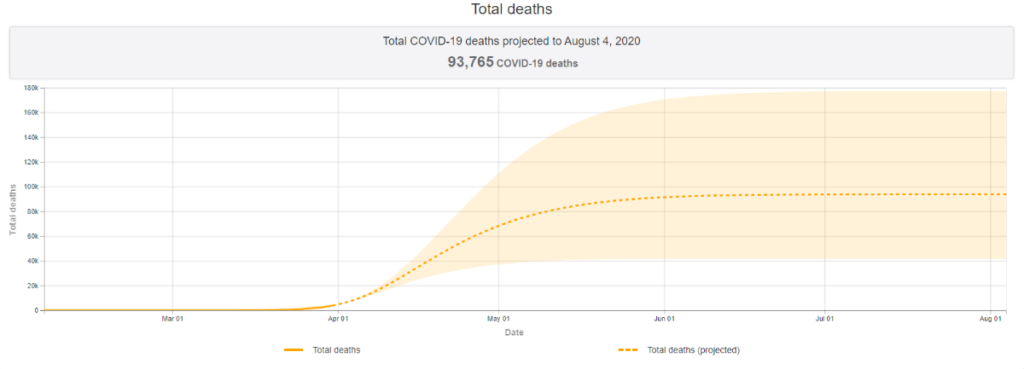
As the virus continues to spread around the world, the U.S. remains the global epicenter. There are now 432,438 reported cases of COVID-19 – more than any other nation and more than twice the number in Spain, the second-hardest hit country with 152,446 cases. Worldwide, as of Thursday, April 9 at 9:00am ET, the Center for Systems Science and Engineering at Johns Hopkins University reported 1,498,833 confirmed cases and 89,733 deaths attributed to COVID-19, including 14,808 deaths in the U.S.
Updated models by the Institute for Health Metrics and Evaluation (IHME) at the University of Washington suggest current diagnoses represent just a fraction of eventual U.S. cases. IHME predicts the epidemic will peak nationwide in just three days, on Sunday, April 12, but state-level epidemics will follow slightly different trajectories. The country could see nearly 60,415 COVID-19 related deaths in the epidemic’s first wave.
Industry Developments
The clinical trials required to prove the safety and efficacy of vaccine and treatment candidates are extensive, and the time to bring these products to market is long. Beyond investments in research and development, pharmaceutical companies are committing extensive resources, both monetary and in-kind, to support the United Nations’ call for an “immediate, coordinated health response.” A comprehensive list may be found here. Select commitments from the past week include:
-
Following the European Medicines Agency’s (EMA) recommendation that Gilead make remdesivir accessible for compassionate use “in a fair and transparent way,” the company announced it is attempting to scale up production to meet demand for clinical trials and compassionate use. Gilead set a goal to produce more than 500,000 treatment courses by October and more than a million by the end of this year.
-
Pfizer announced a commitment of $40 million in medical and charitable cash grants to help respond to the COVID-19 pandemic. Emergency relief funds will be provided to public health agencies and international nonprofit organizations including Direct Relief, International Medical Corps and Project Hope.
-
Medtronic announced it is sharing design specifications for its ventilator to accelerate efforts to increase global production. The current shortage of ventilators, a critical tool in the management of patients with severe cases of COVID-19, is driving innovation in retrofitting and repurposing other medical devices as breathing machines.
-
Johnson & Johnson asserted its potential vaccine against COVID-19 could cost as little as 10 euro per dose. “We are counting on hundreds of millions of people worldwide to have access to this vaccine,” said Paul Stoffels, Vice Chairman of the Executive Committee and Chief Scientific Officer.
-
Recognizing that on-going primary health care needs persist during a pandemic, Merck announced it is donating $3 million through its signature maternal health initiative Merck for Mothers to address maternal health needs during COVID-19. As stated by Julie Gerberding, Chief Patient Officer, “childbirth will not wait for the pandemic to ease.”
-
While President Trump continues to champion hydroxychloroquine, despite lack of clinical evidence, as a potential treatment against COVID-19, the EMA announced it will not clear the medicine for use without trial data. In response to increased demand, Sanofi announced it is prepared to manufacture and provide millions of doses.
From the Experts
“But Covid-19 won’t simply disappear if the wealthy world is left to its own devices, manufacturing costly vaccines that are only affordable to fully insured residents of the 30 richest nations on Earth.”
Laurie Garrett, American science journalist
Thursday, April 2
“Today’s epidemic is a powerful reminder that infectious agents do not respect borders and that global cooperation is essential for dealing with them. Classic public health tools are a must: We cannot control what we cannot understand. And we need to maintain the collaborative and generous spirit that has emerged in response to Covid-19. It may feel like a once in a lifetime experience, but that, alas, is unlikely to be the case.”
Susan Desmond-Hellmann, Former CEO, Bill & Melinda Gates Foundation
Friday, April 3
“This is going to be the hardest and the saddest week of most Americans’ lives. This is going to be our Pearl Harbor moment, our 9/11 moment, only it’s not going to be localized; it’s going to be happening all over the country.”
Vice Admiral Jerome Adams, U.S. Surgeon General
Sunday, April 5
“Africa cannot and will not be a testing ground for any vaccine. We will follow all the rules to test any vaccine or therapeutics all over the world, using exactly the same rule […] to treat human beings the same way, equally.”
Dr. Tedros Adhanom Ghebreyesus, WHO Director-General
Monday, April 6
“Unless the United States exerts leadership to prevent Covid-19 from raging out of control abroad, the crisis will not end at home.”
Samantha Power, former US Ambassador to the United Nations
Tuesday, April 7
“What’s really important is that people don’t turn these early signs of hope into releasing from the 30 days to stop the spread – it’s really critical. If people start going out again and socially interacting, we could see a really acute second wave.”
Dr. Deborah Birx, Coordinator of the White House Coronavirus Task Force
Wednesday, April 8
Additional Resources
Reports from International Governments and Bodies
-
Shared Responsibility, Global Solidarity United Nations Report on Responding to the Socio-economic Impacts of COVID-19
-
White House Coronavirus Task Force Press Briefings, April 6, April 7, April 8
Funding and Policy Trackers
Academic and Market Research Literature
Communications Toolkit
What We’re Reading
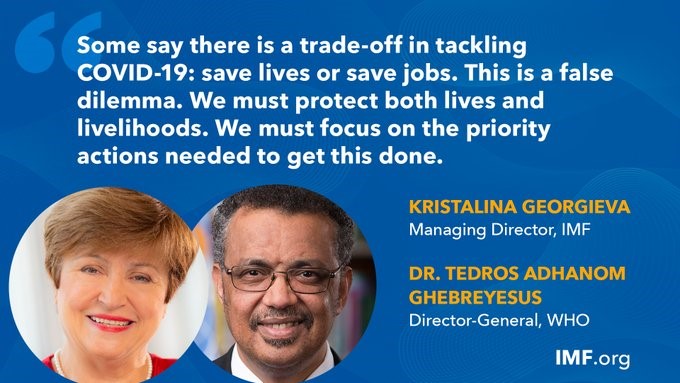
Some say there is a trade-off: save lives or save jobs – this is a false dilemma, Kristalina Georgieva and Tedros Adhanom Ghebreyesus, The Guardian
Virus exposes glaring inequalities between rich and poor, Winnie Byanyima, Business Day
Early Data Shows African Americans Have Contracted and Died of Coronavirus at an Alarming Rate, Akilah Johnson and Talia Buford, ProPublica
Redefining vulnerability in the era of COVID-19, Editorial team, The Lancet
COVID-19 will not leave behind refugees and migrants, Editorial team, The Lancet
Preparing for the Next Pandemic, Susan Desmond-Hellman, The Wall Street Journal
More herd immunity, less herd mentality, Ariel Pablos-Méndez, The Hill
Managing the march of COVID-19: lessons from the HIV and AIDS epidemic, Alan Whiteside, Warren Parker & Mike Schramm, African Journal of AIDS Research
This Won’t End for Anyone Until It Ends for Everyone, Samantha Power, The New York Times